Part One: What on Earth am I doing to myself?
Part Two: Making Tough Decisions
A lot of you have been chasing me for Part 3 of this series of blogs. Unfortunately this has been, by far, the hardest piece for me to write – not just because it covers what the trial involved but also because of what happened in my personal life during the course of the trial. So it’s safe to say this isn’t my first attempt to get these thoughts out, the second or even the tenth.
I endeavour to do my best to separate the treatment and my personal life but, as you can imagine, the two bleed heavily into each other so please forgive me in advance.
Clinical Trial: Day One
The first day of the trial was pretty intense and I ended up taking my Dad with me to support me as the first day involved not only an MRI but several assessments as well as my first rTMS session. I probably could have done it myself but physical weakness and anxiety meant it felt safer to have support at hand. I would recommend others take someone with them as it is quite long and can be quite an exhausting experience. Dad was quite chuffed about coming along, especially as he has a background in scientific imaging and is a Kings College London Alumni. As a student he lived just across the road from where I was being treated (which meant he could revisit old haunts including his houses of residence and places him and my Mum used to go when they first met).
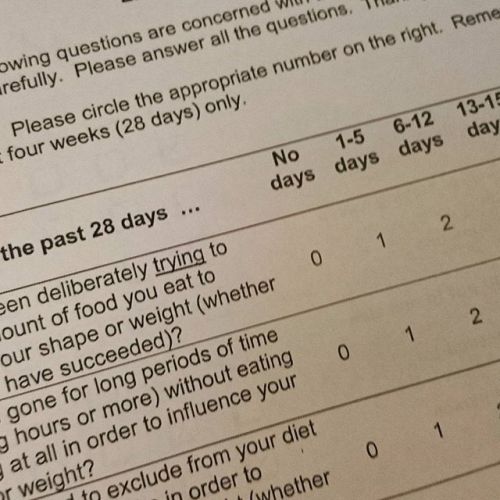
We arrived at the IoPP Neuroimaging department after catching a very early train – the staff I must say were absolutely lovely, all of them. After filling out more paperwork I was ushered through to an area where I could remove any and all metal items and store them and my bag in a locker.
Thankfully, to my surprise, there was no voyeuristic hospital dressing gown and I was allowed to wear my own clothes.
The people who operate the MRI were absolutely lovely, I couldn’t fault them. I wasn’t nervous but I was bloody freezing and they put pillows under me and a blanket over me to keep me warm and talked to me throughout the procedure to keep me at ease and make sure I was OK (and warm enough).
Having an MRI scan
The MRI itself was quite an experience – I had previously only witnessed them on TV and as it turns out, watching all eight series of House does not give you a realistic idea of what to expect.. who knew?
I was under the impression that they were a tad scary and made one particular noise over and over again. As it turns out MRIs make such a wide array of noises it’s almost as though they have their own language – whirring, beeping, buzzing and banging depending on where they are looking in your brain and what they are doing.
For the first part I had a couple of calibration tests followed later on by a fuller set of basic tests. I was surprised at how close I came to falling asleep during the more restful period where I didn’t have to do any tasks (admittedly throughout the whole process but especially this bit) – I had assumed sleep would be impossible in such an environment but apparently it’s quite common. Unfortunately the end was the more active part otherwise I would definitely have had a cheeky nap!
After an hour in the machine I did several basic assessments that looked at my perception of the healthiness and tastiness of various foods and then we were ready for session one.
The First rTMS Session – What to expect
The first session was a bit daunting but I was put at ease at every stage of the trial in fact with the absolutely lovely researchers I worked with.
Sessions started with a quick computer task which was essentially watching food videos – for me this actually the worst part of the entire trial! I realise a lot of people with Anorexia LOVE food (believe me you should see my social media feeds during Great British Bake Off). I am indifferent to food at best, repulsed at worst and so even 90 seconds of these videos a day were enough to cause my anxiety to leap and appetite to drop. This was preceded and then followed by some quick measures on how full I felt, how anxious etc.
A calibration test was done for the machines to try and work out where a specific itsy-bitsy part of my brain was (the motor cortex). This is not always an easy task and the researchers explained that it can take many attempts to find it and even then sometimes you just don’t.
This calibration happened on a weekly basis and it was interesting that some weeks it was easy to find and others were like looking for a needle in a neurological haystack!
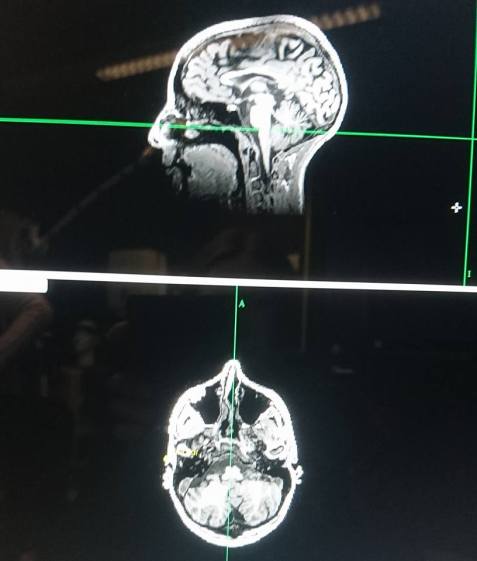
Check out my beautiful brain!
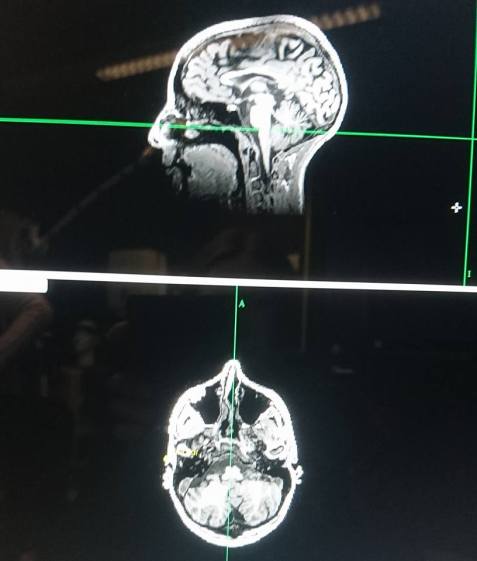
This is what I have started referring to as my “brain selfie”!
This test is done to make sure that the “coil” they use to deliver the TMS is positioned correctly – what they are actually looking to stimulate is part of your pre-frontal cortex which is part of the brain that controls mood regulation among other things.
This is what the coil looks like when it is on your head – it’s quite something! Personally I’m not sure this particular fashion trend will take off..

What does rTMS feel like?
As much as the researchers had tried to explain what it felt like (they had all undergone sessions so had personal experience) it is still a bit different for each person. It also can take a higher “dose” to get the required effect in some patients or even session to session which then further affects variation of experience.
For me I didn’t find the sensation painful, it was probably best described as uncomfortable. With each set of “pulses” sent out there were quite loud clicking noises. As it was on my head I felt something akin to a strong set of vibrations (again not painful). It also made my jaw shake uncontrollably because of these vibrations so I tended to keep my mouth shut (shocking I know!) while the pulses were delivered otherwise I ended up with chattering teeth and I sounded pretty ridiculous!
Side effects of rTMS
Sessions varied in how they left me feeling and the side effects I encountered. The main side effects I experienced were:
- Headaches
- Eye strain
- Nausea
Other people have been known to experience other side effects including:
- Light headedness – admittedly I did get this but as someone with low blood pressure and other co-morbid conditions this is fairly normal for me so I wasn’t able to work out if this was made worse by the treatment
- Discomfort on the scalp
There are some more serious side effects but these seem to be very uncommon.
During the earlier sessions I definitely experienced more headaches and eye strain but this lessened over the following sessions, perhaps because my body was becoming more acclimatised? The eye strain also lessened if I wore my glasses straight after the session for a few hours (usually I just wear them for reading).
I also experienced quite high levels of nausea (although no vomiting thankfully). I am very aware that nausea is my body’s go-to reaction to a lot of treatments (mostly previous experiences with medication) so it’s likely I was always going to have a slightly more extreme experience in this regard. I found if I ate something small and very bland (say crackers) a few hours before the nausea would be pretty bad but not unbearable but if I did eat something richer it made me worse. But that’s just me and I would never endorse restriction obviously.
Devious Anorexia and Self Sabotage
As I mentioned in part two of this series of blogs, one of my main concerns would be how my Anorexia might try and sabotage me during the trial. I was very aware that this was the most freedom I had been given in over a year and freedom is a dangerous thing when you can’t trust your mind. I wanted so badly to prove that I could handle this level of freedom and this change and be trusted but the voice was so, so strong every hour of every day.
Unfortunately some of my fears were realised although things never got to the point where they jeopardised my place on the trial (e.g. dropping under the minimum weight requirement) and I managed to stay just above water long enough to undergo the whole course of treatment.
On reflection my Anorexia did use the trial as a means to restrict my diet to some extent and vastly increased the amount of exercise I was doing (mostly because of the walk to and from the station and when trains arrived early and I had time to kill). It was also very easy to slip back into the deceit: “have you eaten?” (yes but really no), “did you relax at the coffee shop when you arrived?” (yes but really no I walked for miles), “do you want a lift home from the station?” (yes because I’m exhausted but no because I can’t fight the urge to exercise).
Going through the trial without any external professional support was not good for me. I wish the team I was under had the foresight to realise that and to actually give me what I had been promised – sessions during the treatment to support me. However due to various issues and miscommunication I didn’t get a session until after the treatment was long done which ended up feeling utterly pointless.
Do I feel any better after rTMS?
Unfortunately the simple answer is: no.
I find out in a matter of days whether I was in the real or placebo group and I am desperately hoping it was the latter. Not because I want to spend another month of my life commuting and having my brain zapped (it’s exhausting, expensive and time consuming) but because if it was real it didn’t work (at least it feels that way right now)..and that’s another option crossed off, leaving me with very little, if any, options left for treatment.
HOWEVER this answer comes with an absolutely huge caveat – and that is what happened during the trial in my personal life which undoubtedly had a profound and disastrous impact on my mental health. If it was the real treatment it could well have not worked to it’s full extent because of everything else that was going on. I don’t know.
The personal stuff
Friends, family and readers of this blog will know that life for me and my partner has been very difficult for a long time now. To sum things up far too briefly in the last few years we lost our home and ended up moving back in with my family after 7 years away, we both got made redundant and we lost my partner’s grandfather in September 2016 after a long and bitter battle with Dementia. On top of our existing mental and physical health issues of course.
So as you can imagine things weren’t great. We struggled along on my benefits and the incredible and unconditional love and support of our parents but it was hard.
And then our world came crashing down.
Not long into the trial we discovered that my partner’s father had Cancer. Less than a week later we were told the worst news I have ever heard; it was Stage 4, it had spread, there were no treatment options, it was terminal.
Obviously this was absolutely devastating for absolutely all of us. And a complete shock. We walked around in a daze, we tried to comprehend, we still can’t. I won’t go into too much detail, it’s not my story to tel but I can talk about how it affected me in the immediate aftermath to give you an idea of how much my world was rocked during treatment and how this may have impacted on it’s efficacy.
I cried every day for weeks. Multiple times a day. Even in public (if you know me you know this DOES NOT HAPPEN). I cried five times just on the way to treatment one day when train delays pushed emotions over the edge and ended up literally collapsed, on my knees, hiding behind a pillar outside Blackfriars Station bawling my eyes out. I gave up on trying to hide it. I cried in public toilets, on the train, walking down the street.
Months on, now we find ourselves in the new year and the weeks are flying past I try desperately to work out what’s what – how am I feeling? What is causing it? Do I think the treatment worked? Was I even in the treatment group or did I get the placebo? It feels impossible to untangle.
So I’m sorry because I know this is not a neat story.
I wish I could say “I have struggled for years but after a few sessions I felt great!”. I wish I could be one of those inspirational “sick to picture perfect recovery”, “before and after” features but my life is not and has never been like that.
I will find out imminently whether I had the real or placebo sessions during the trial. I am completely unsure how to feel about this and I must admit a large dose of apprehension. If it was real and I’m no better that feels like yet another door closing on my already badly bruised face and if it was the placebo I have to muster up the motivation and energy to go through the process again, this time for real.
So watch this space for the results, honestly it’s going to be as much a surprise to me as it will be to you.