Well it’s been another whirlwind of a year, it seems to have flown by at breakneck speed and all of a sudden it’s the end of 2014 and I’m wondering what I’ve actually done this year.
For once it’s been no surprise that the year has flown, it’s been busy after all and I’ve done quite a lot. In fact this year I’ve not only started a new job but also moved house and been on the holiday of a lifetime. And that’s on top of my usual way more than 9-5 with some volunteering and a lot of campaigning thrown in for good measure.
So here’s a bit of an overview of my year which will be followed by a blog summing up some of my heroes of 2014.
January
2014 didn’t get off to the best start as I ran around the town I was living in and London desperately trying to get ahold of some medication. Being on long term medication feels like second nature after all the years and it does go along way to levelling me out and keeping me functioning but definitely has it’s downsides. Being on a relatively unusual medication and trying to get a GP appointment near Christmas and while working full time is not a good combination and I still manage to mess up my planning from time to time.
It did get considerably better thankfully, January was the month my Chrissy B appearance talking about growing up with mental health issues was aired.

I also found time for my parent’s annual Burn’s Night party at the end of the month which was, as usual completely tartan and tasteless and a good way to celebrate the end of a very long month.
February
In February I finally got a chance to do Mental Health First Aid training with colleagues from NHS England. I think it’s great that my employer gave us all the chance to do this course and, upon competition, publicised the fact the office now had both physical and mental health first aiders. As many mental health issues surface or are even caused by work I’d love to see more workplaces taking this step. It was also an opportunity to bond with colleagues, many of whom opened up about their own experiences.
I also had the opportunity to co-facilitate a special online talk for the sadly now defunct MindFullUK during Eating Disorder Awareness Week. Having spent a few years now doing something similar for YouthNet on a regular basis it was interesting to try this method with a new group of young people.
March
As the NHS Expo was held in Manchester this year I had a great excuse to start the month of March with friends Rachael and Claire and their assortment of rats.
March was also pretty amazing in that I was given a regional award at the Vinspired Awards in the “Most Outstanding Social Entrepreneur” category for my work on the WellHappy app. I even got to attend a fancy awards ceremony at the 02 with my partner Ryan, parents and colleagues from myhealthlondon.

Boyfriend looking quite proud don’t you think?
April
In April I had the opportunity to speak to the Clinical Senate at the Kings Fund about young people, mental health and technology. Even though it’s a talk I’ve given so many times I could probably recite it in my sleep I received an inordinate amount of praise for this one. It got me thinking about the audiences I tend to speak to; usually a group of people who have signed up because they already have an insight and interest in what I’m speaking about, in other words, preaching to the converted. This is something that’s troubled me a lot this year; how do I reach a broader audience including some of the sceptics and naysayers?
I had the opportunity to learn a huge amount when I received Dementia Friends training from Katie Nichol and since then have, unfortunately, had the opportunity to put this learning into practice. I’d recommend the course to everyone as Dementia is something we will all be affected by at some point in our lives.
I also got a chance to attend the launch of the YoungMinds HedMeds project which had been something of a labour of love and personal interest for me. Along with a dear friend, Annabelle, we opened up the event and even preceded Jo Brand who very kindly called us a hard act to follow!

Some of us with Dr.Ranj
May
May was a big month that began with me presenting at the Patient Information Forum conference alongside Macmillan.
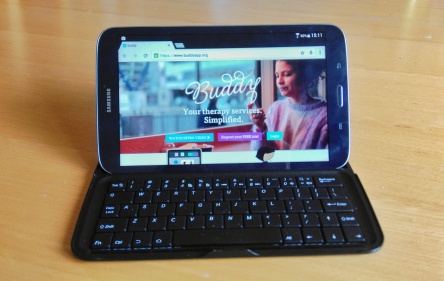
This was followed by an interview for my current role at BuddyApp..the beginning of big changes.
Then the biggest media appearance of my life, a live slot on Newsnight to talk about self harm with myself and Tanya Byron taking on the legendary Jeremy Paxman. I was approached by YoungMinds and asked if I would like to appear..only a few hours before broadcast. It was probably one of the most surreal moments of my life to be sat in the BBC green room and having a chat with Mr.Paxman.

I am very used to being on the receiving end of calls for help, queries, comments and young people generally asking for help and advice but this has increased by an order of magnitude since my appearance. As I may have mentioned these messages usually start with the same phrase, “I’m really sorry but I don’t know who else to talk to”. While I’m glad that I’m seen as approachable it does sadden me that young people still struggle to find people to trust and open up to and how few positive mental health role models that they can easily access there are.
June
In June I received some good news about my health when I learnt that, by some miracle, my bone density is still at a reasonable level, certainly better than I could have hoped for. Throughout the year I’ve had countless run ins with the medical world from a personal perspective, thankfully most of them positive.
June was also the month where I prepared myself for leaving the NHS and my lovely team at myhealthlondon. This was bittersweet, I was going on to a fantastic new role but leaving so much behind. Having worked in the NHS for 18 months I learnt so much about what happens “on the inside” and it gave me a really helpful perspective for when I’ve got my service user hat on and am wondering why things aren’t happening the way I had hoped in my treatment. I also met the most amazing people during my time working for the NHS, too many to name here, and thankfully I’ve managed to stay in contact with most of them.

I’ve argued for a long time that the people who work for the NHS are some of the best people you will ever meet, their kindness, compassion and work ethic can be incredible but they are bound by a system that can be slow, bureaucratic and seemingly impossible to navigate so it’s no wonder things don’t always work.
Something that really fascinated me during this time was the way the NHS is perceived by both the general public and the media.
I feel as though people see the NHS as one big, monolithic organisation, especially when they are commenting on their experiences, “The NHS did this/didn’t do this” etc. This is a serious misunderstanding as the reality is the NHS is a jigsaw (and the pieces don’t necessarily fit well), made up of hundreds of different providers and a huge number of staff. In fact the NHS is the biggest employer in Europe and can be almost impossible to navigate..even if you work in it.
Throughout my time in the NHS we also noticed a change in the media’s attitude towards us. It got to the point where everyday there was a new story coming out, almost all negative and this has a huge effect on staff morale as you can imagine. And yet when we reached out to the media to get good news stories they were passed up time and time again. Bad news may sell more papers but it’s disingenuous and can be downright dangerous in painting an unrealistic picture that scares people off and causes them to lose faith in what is still an incredible British institution.
Obviously I have had a huge range of experiences having used NHS mental health services in particular on and off for a decade. Some have been great, some terrible but it’s been a spectrum and I can’t just focus on one end. I also look at countries like the USA and think about how terrifying it must be to have to pay so much for what I would argue is a basic human right; the right to life. I look at my friends who have poor or no insurance and gasp in horror at their medical bills festooned with zeros and wonder what my own care has cost and wonder where I would be if I had been born on that side of the pond.
July
On the 1st of July I started my new role at BuddyApp. This has been such a huge but positive move for me. I left one of the world’s largest organisations to go work at a start up with less staff that I could count on my fingers and of which I am the only female so that was quite a shock to the system.
I can honestly say that working at Buddy for the last six months has been a pleasure and I have particularly liked working in a small, dynamic team and the chance to work on the edges of the NHS, working directly with front line staff.
There have been challenges certainly, getting the NHS to buy into and embed something innovative is a slow process, definitely more of a marathon than a sprint, but it’s worth it. Because when it does work, we help patients get better and support clinicians in doing their job, what could be better?
So July was mainly spent settling in, meeting colleagues and clincians for the first time and a few events thrown in for good measure. My favourite was probably the NHS England Youth Forum’s “Celebrating Positive Youth Mental Health” event which I attended with Miranda Bunting whose blog you can read here.
August
In August I took part in another Cormack family tradition; Cropredy festival. Big events can be a challenge for me especially when it comes to my anxiety but last year I decided that this would be the one weekend every year when the mental health issues would just have to sit in the backseat and sulk. This year I kept this resolution going and had a great time as you can probably tell from this picture of me and my brother.

Sadly August was somewhat marred by ongoing issues in our housing situation, most notably problems with our neighbours. Having moved into our flat two years previously and built a wonderful home for ourselves, my partner and I found the last year unbearably stressful due to issues next door which culminated in a police raid-a pretty traumatic experience for anyone.
For me a home should be somewhere that you feel safe and by the time we decided to get the hell out of dodge this was no longer the case. It has been a huge step and at times a bitter pill to swallow but, for the sake of our sanity, we left and moved in with my parents.
After 7 years away from my hometown it’s obviously taken time to adjust but I’m lucky that I still have some great friends in the area and above all a ridiculously supportive family who have taken in both myself, my partner and our ridiculous and noisy cat. It makes it easier knowing that this is a temporary solution and I’m grateful to have this time to settle, relax and rebuild.
September
September was dominated by the holiday of a lifetime as me and my family embarked on our Trans-Siberian Railway adventure. There’s definitely an entire blog post to be made out of this at some point considering we crossed China, Mongolia and Russia in 16 days and saw and experienced so much I don’t even know where to start. As someone who commutes 5 days a week as it is the idea of being on a train for the lion’s share of a fortnight initially didn’t appeal much but believe me the tube and this experience just don’t compare.

Rocking my YoungMinds Vs tshirt on the Great Wall of China
Some highlights include seeing the Terracotta Warriors, standing on the Great Wall of China in my YoungMinds Vs tshirt, drinking the water of Lake Baikal and being chased around China by people who had never seen redheads. I think my brother, all 6 foot of his bearded, tattooed and pierced self was a bit much for some of them. My brother was a bit bemused by this too, as well as many of the tshirt slogans we saw.

Upon my return the rest of September was mostly spent given presentations at The Kings Fund, Westminster Briefing (The role of technologies: what young people want from services today) and attending the NHS AGM and NHS Citizen event where I may have caused a bit of a stir by wearing a protest t-shirt from 38degrees on stage with the NHS board of directors..oops..
October
In October I went to the launch event for the London Health Commission Better Health for London report which was held at the House of Lords and involved a lot of alcohol (how the other half live!).
The highlight of October and in fact one of the top events I took part in during 2014 was CLASP’s Walking Out of Darkness event. Over 300 of us descended on London for a 10 mile walk to raise awareness and funds for mental health and in particular, suicide. We raised a staggering £30,000 and are already planning the next event, you can join us on May 16th and raise money for whichever mental health charity you choose.

I also became a trustee for CLASP and have had the pleasure of working with the CEO and founder of CLASP, Kenny Johnston.
November
November truly felt like conference season was underway with me speaking at both Health 2.0 and HANDI Health Apps during EHILive about Buddy app including my experiences of using Buddy in my own treatment.
I also filmed a short piece for Techforgood.tv which you can now see here.
On top of a lot of travelling during the month I also found time to attend the Social Enterprise UK Awards around the corner from our office in Old Street. It was great to do something fun with my colleague James Ryan and I loved the atmosphere, social entrepreneurs in the UK are a fairly close knit and very supportive bunch and I’ve really enjoyed entering this world in 2014.

December
Far from winding down towards the end of the year it feels like there was even more going on than usual during December.
I gave a presentation at UCL to Clinical Psychology students about the pros and pitfalls of peer support and social media for people experiencing mental health issues. During this I was reunited with the fabulous Tanya Byron who I shared the screen with during my Newsnight appearance. I also had the chance to have a sneaky drink with the lovely Grace who I know from VIK days, I think the students were a bit surprised to see me in their bar after the talk but it was the last day of term so I blame getting caught up in the atmosphere!
I also sat down with young people from YoungMinds Vs project (the next and very exciting generation of activists, definitely worth checking out) and Norman Lamb to discuss youth mental health, you can find more information from our afternoon with the minister here in a great blog written by two of the young activists.
On a personal note the most touching experience I had this month was helping out one of my role models Monique-Amy Newton in her annual “Help the Homeless” event. Sadly I was only able to attend one evening but we gave out clothes, food and toiletries to a large number of people both on the streets and in hostels. Their gratitude for a bowl of soup or pair of gloves was humbling and really put my own life into perspective.

TL; DR: Overall it’s been a whirlwind of the year. I’ve had some of my greatest experiences and biggest challenges. I’m very thankful to have some time off between now and 2015 when it all starts again. Hopefully onwards and upwards to better things.
Thank you so much for everyone who has supported me this year, it has meant the world. I’ve stayed in contact with some great people and met some truly inspirational movers and shakers in the health and social care world. It’s people like these that give me the courage to keep going, keep standing up for what I believe in and keep fighting the good fight.
A particular thank you to my family, the never ending support of Ryan Jackson and a particular thanks to two ladies who have had me both in tears of laughter this year, founder of Diabetics With Eating Disorders (DWED) Jacq Allan and Kat Pugh who runs the wonderful #EndTheWait campaign for earlier intervention in Eating Disorders. I’m very lucky to be surrounded by powerful, disruptive, caring female role models.